|
TOTAL HIP REPLACEMENT
A Guide for Patients
The Basford Consulting Rooms has a number of Orthopaedic Surgeons who specialise in Hip Replacement Surgery.
Introduction
This booklet provides information for you and your family regarding total hip replacement. Your Consultant may recommend a total hip replacement for you, but the decision to have the operation is yours. Your decision must be based upon weighing the benefits against any risks. If you have any questions as you read through this booklet then ask the doctor, nurse or therapist at your next visit. You may find it helpful to make a note of your questions before you see the doctor or nurse.
What Is A Hip Replacement?
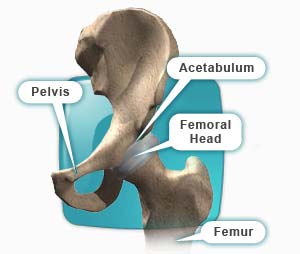
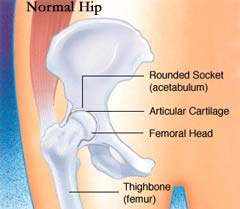
A Total Hip Replacement is a surgical procedure in which damaged parts of the hip joint are replaced with an artificial joint (prosthesis).
During the procedure the ball and socket joint that joins the pelvis and the thigh bone (femur) are removed.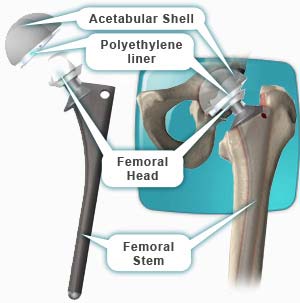
The artificial hip itself is made up of two parts, a cup like device that fits in the hip socket and a metal stem
with a metal ball on the top which is inserted into the thigh bone (femur). These new parts allow your new hip
to move. There may be other options which your Consultant will discuss with you.
By replacing your worn hip joint with an artificial joint, hip replacement surgery can relieve your pain and help you to get back to enjoying
normal, everyday activities again.
Why Have A Hip Replacement?
 Osteoarthritis is the most common reason for a hip replacement. Osteoarthritis is a degenerative disorder often referred to as wear and tear arthritis. Osteoarthritis is the most common reason for a hip replacement. Osteoarthritis is a degenerative disorder often referred to as wear and tear arthritis.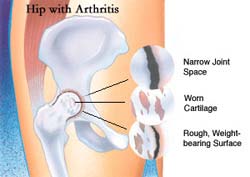
However, there are many other types of arthritis such as rheumatoid arthritis, which is caused by inflammation in the joint.
Your consultant will often try simple conservative measures such as physiotherapy, weight loss, anti-inflammatory tablets and pain killers to control your pain before opting for surgery.
 When your arthritis becomes so severe that the pain wakes you at night or your joint movement becomes limited, preventing you from walking any distance, your orthopaedic consultant may recommend surgery. When your arthritis becomes so severe that the pain wakes you at night or your joint movement becomes limited, preventing you from walking any distance, your orthopaedic consultant may recommend surgery.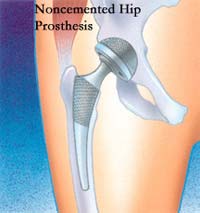
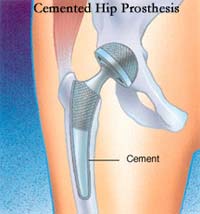
There are various types of hip replacements and, broadly, they can be divided into cemented and non-cemented replacements.
Various types of articulating surfaces are also used.
Your surgeon will explain the various options and the reasons for a particular preference in your case.
How Successful Is A Total Hip Replacement?
 Results are normally very good. Most patients are relieved of their hip and groin pain. As the pain lessens, range of movement also improves. Most patients can walk further and limp less. 90% of total hip replacement joints will last for 10 years or more. Results are normally very good. Most patients are relieved of their hip and groin pain. As the pain lessens, range of movement also improves. Most patients can walk further and limp less. 90% of total hip replacement joints will last for 10 years or more.
How Long Do Total Hip Replacements Last?
Hip replacements do eventually wear out. The major long-term problem is loosening. This occurs because the cement crumbles (as old mortar does in a brick building) or the bone melts away (resorbs) from the prosthesis.
When a hip replacement does wear out it can be revised. The results of a second operation (revised hip) are not as good as the first time around. This is why your doctor will often try and delay your first operation for as long as possible.
Loosening in part is related to your weight and activity. After your operation it is important to control your weight and avoid excessive amounts of exercise such as jogging.
You are at greater risk of loosening if you have osteoporosis.
Are There Any Risks Involved?
Yes, all surgery and anaesthesia involves some risk. The health team looking after you will try and make you as fit as possible before surgery to minimise any risks.
Some people are more at risk of complications than others are. For example overweight patients are more at risk of wound and anaesthetic problems, patients with rheumatoid arthritis and diabetes are more at risk of infection and patients with poor muscle control such as epilepsy and Parkinsonís disease are more at risk of dislocation.
The most common complications are:
Deep vein thrombosis or D.V.T.
DVT is a blood clot in the veins of your leg. Occasionally the clot can dislodge and travel to the lungs (pulmonary embolus). The chances of this happening are very small. To help avoid thrombosis the physiotherapists and nurses will get you moving around as soon as possible, usually on the day after your surgery. You will be given blood-thinning medication to prevent blood clots forming and you will also be measured for special elastic anti-embolism stockings on admission. These help increase the blood flow in your legs and they are usually worn for six weeks after surgery.
Infection
A very small number of patients develop an infection. Usually these clear up quickly with antibiotics. Some infections like MRSA are resistant to common antibiotics and therefore more difficult to treat. At the Pre-operative Assessment we screen for MRSA by taking swabs from the nose and skin of all patients coming in for elective surgery. MRSA can be treated before admission. To reduce the risk of infection the theatres are equipped with a special filtered ventilation system; you will be given antibiotics intravenously while you are under the anaesthetic; and all the wards have alcohol gel dispensers to help provide better hand hygiene and prevent cross-infection between patients.
Dislocation
This happens when the ball comes out of the hip socket. If it happens in the first few weeks after the operation it is usually due to instability while the muscles are still healing. The nurses, occupational therapists and physiotherapists will teach you how to protect your new joint and avoid activities, which increase the risk of dislocation. If you have repeated dislocations sometimes the hip operation has to be revised.
Anaesthetic risk
You will be seen in the assessment clinic for a health screen and your anaesthetist will also see you before your operation to discuss the anaesthetic choices available.
The choices are general anaesthetic, spinal anaesthetic or a combination of epidural and general anaesthetic.
Your anaesthetist will be able to advise you which technique might be more suitable for you, taking into account your general health. They will also advise you of any other special techniques, which might be necessary for you, and give an indication of any particular risks regarding your general state of health.
Leg length inequality
The surgeon will make every effort to maintain the length of the leg but there is no guarantee. When you start walking you may find your leg feels longer or shorter. This usually resolves once the swelling from surgery goes down and your muscles get stronger.
Nerve injury
The sciatic nerve at the back of the hip and the femoral nerve at the front of the hip are at risk of damage during the operation. Nerve damage is fortunately very rare but it can occur even if the nerve is not actually cut.
Getting Ready For Your Operation
It is important that you are fit for your operation, as you will make a quicker recovery.
If you smoke, try to cut down or quit. Smoking changes blood flow patterns, delays healing and slows recovery. If you want to stop smoking ask for information about the Smoking Cessation Nurse.
Keep your weight down. Being very overweight (i.e. a Body Mass Index of greater than 30) can significantly increase the risk of complications from surgery and anaesthesia. The Assessment Nurse will weigh you and measure your height and give you some advice. You may find it helpful to talk to your General Practitioner or Practice Nurse. If you are seriously overweight your Surgeon may need to delay surgery until you have lost some weight.
Have a dental check if you have not done so in the last six months. It is important that any dental infections are dealt with before joint replacement surgery to prevent infection of your new hip.
Practice sleeping on your back - you will not be allowed to lie on your side for approximately six weeks following surgery.
Start some gentle exercises according to advice from your doctor or physiotherapist. These may be uncomfortable at first but gentle exercises help the muscles around the joints become stronger and reduce stiffness. They will also aid your recovery following surgery.
Foot rotation - whilst sitting in a chair with your back supported, raise your leg so that your heel is off the floor. Circle your foot clockwise ten times and then circle your foot anti-clockwise five times. Now try your other foot. Increase the number of times you rotate your foot each time you exercise.
Foot flexion - sit in a chair with your back supported and both feet flat on the floor in front of you. Raise both heels off the floor so that the balls of your feet are touching the floor.
Lower your heels slowly, and then raise your toes so that this time only your heel is touching the floor. Again lower slowly. Repeat five times; increase up to ten times, as the exercise becomes easier.
Leg raises - sit in a chair with your back supported. Raise your right leg from the ground to the level of your knee or as far as you can manage whilst keeping your thigh in contact with the chair. Hold your leg raised for five seconds then very slowly lower it back to the floor. Repeat this five times. Now try your other leg. As your muscles get stronger try keeping your leg raised for longer.
Before Your Operation
Hip Education Group
You may be asked to attend an education session about all aspects of your operation, hospital stay and recovery, which lasts for about an hour and a half on a Thursday afternoon. You can bring someone with you if you wish. You will meet one of the Pre-operative Assessment Nurses, a Physiotherapist and a member of the Occupational Therapy team, and have a chance to ask them questions.
Pre-operative Assessment
A couple of weeks before your operation you will also be asked to attend a Preoperative Assessment Clinic where you will undergo routine investigations such as blood pressure measurement, blood tests and heart tracing.
Please bring your tablets, inhalers and any other medicines you take. If you take medicine for high blood pressure it would be helpful to bring some recent blood pressure readings. If you are diabetic please bring a record of your blood sugar readings. If you are on Warfarin please bring your yellow book. Late cancellations waste operating time and lengthen the waiting list.
Plan Ahead For Your Homecoming
Getting the full benefit from hip replacement surgery can take a few months and during this time a full range of movement may be difficult. As a consequence many people find they are limited in their ability to do normal activities such as bathing, shopping, laundry, cooking and housework. Help from others may be needed.
It is important to plan ahead and think about the support you will need when you go home, usually at around five days after surgery.
Here are some suggestions to start thinking about:
Arrange for someone to take you home from the hospital. You will not be allowed to drive for six weeks after your operation.
If you are caring for someone else you will need to make alternative arrangements for their care (respite, home care, help from friends or family)
Is anyone available to help you when you come out of hospital? It is better if someone can be with you for the first week or two following discharge to help with things like cooking and personal care, if only for part of the day. If you do have any concerns about going home please discuss them with the Assessment Nurse.
It is a good idea to prepare and freeze some meals in advance or arrange for relatives and friends to bring meals.
Organise your kitchen to avoid excessive lifting and bending. The Occupational Therapist can advise you on the use of equipment to assist 
you in the kitchen.
Remove any rugs that could cause you to trip. Securely fasten any electric wires and ensure a safe passage throughout your home
Will I Need Anything Special At Home?
 The Occupational Therapist (OT) will assess your requirements and order appropriate equipment to help you once you are back home. You will be asked to provide information about your home environment and how you are coping at home prior to you The Occupational Therapist (OT) will assess your requirements and order appropriate equipment to help you once you are back home. You will be asked to provide information about your home environment and how you are coping at home prior to you r admission, usually at the Pre-operative Assessment Clinic. The Occupational Therapist will advise you how r admission, usually at the Pre-operative Assessment Clinic. The Occupational Therapist will advise you how
to carry out activities of daily living without excessive bending. They will also discuss managing everyday activities 
safely after hip surgery.
You will require a suitable armchair. The Occupational Therapist will advise you on the height of the chair. It must not be too
low, soft or deep. You should be able to get out of the chair easily without bending your hip at more than a right angle. Chairs
without arms should be avoided initially. Swivel office chairs and manually reclining chairs are not recommended.
Depending on the height of your toilet seat you may require a raised toilet seat for at least 6 weeks
When Will I Be Admitted To Hospital?
Usually you will be admitted to the Ward on the day of your operation.
Please only bring on admission what you will need for the first couple of days such as medication, toiletries, nightwear, glasses etc.
Before you go to theatre:
A member of the medical team will mark the limb to be operated on
Your anaesthetist will meet you and discuss the types of anaesthetic and pain relief available
It is essential that you do not have anything to eat, drink or chew for some hours before your operation, as this could cause vomiting while you are under the anaesthetic
You will have a shower and change into a hospital gown. You will be asked to remove any make-up or nail polish and all jewellery except for a wedding ring.
You will be transported to theatre in your hospital bed.
What to Expect After Surgery
After surgery you will be monitored closely while you wake up from your anaesthetic. When you are awake you may go to the Extended Recovery Bay.
Every effort is made to ensure your comfort and safety. This means that you will have your blood pressure, heart rate and oxygen levels monitored throughout. You will have a drip in your arm to ensure you get enough fluids. You will be able to have a drink a few hours after your operation has finished providing that you do not feel sick. If sickness is a problem, anti-sickness medicine will be given to you. You will be able to eat as soon as you feel like it.
You will have drainage tubes in your wound to prevent any bruise forming and to collect any blood loss. Sometimes this blood loss is collected, cleansed - with a machine called a Cell Saver - and re-infused to you through the drip. Some patients require a blood transfusion. You will be given oxygen through a mask for a few hours.
You will be required to lie on your back after your operation with a pillow placed between your knees. This is to protect your new hip and make sure it stays in the right position.
It is recommended that you bring a small overnight bag containing toiletries into hospital to take with you to the Recovery.
Pain Management
You will have some discomfort or pain after surgery. The nursing staff will assist you to control any pain through injections or tablets.
 Your anaesthetist will discuss the best method of controlling your pain with you. There is a form of pain relief available called a PCA (Patient Controlled Analgesia). This means you will have a pump, which you control yourself to administer small doses of painkiller by pressing a button on the handset whenever you need more pain relief. It is very safe and you will be closely monitored by nursing staff. Your anaesthetist will discuss the best method of controlling your pain with you. There is a form of pain relief available called a PCA (Patient Controlled Analgesia). This means you will have a pump, which you control yourself to administer small doses of painkiller by pressing a button on the handset whenever you need more pain relief. It is very safe and you will be closely monitored by nursing staff.
Another form of pain relief is an epidural. The anaesthetist inserts a thin hollow needle into the epidural space, just outside the outer covering of the spinal cord in the lower back. A small plastic tube is then introduced through the needle and left in position when the needle is removed. The tube is used to introduce local anaesthetic and pain killing medication. Staff will be happy to help you in any way to make your stay as comfortable as possible.
On the first day after your operation you will be shown how to get out of bed by your Physiotherapist. They will show you the correct way to move safely. You will also be shown exercises to regain movement and strength in your hip. You will be expected to carry out your own exercises and practice walking once the physiotherapist decides it is safe for you to do so.
Doís And Doníts after Surgery
Everyone heals at different rates, so you may find you are able to carry out some activities fairly quickly following your operation. Provided this does not cause any pain or discomfort you can continue with caution.
Remember if an activity causes you pain - STOP - itís obvious your new hip is not ready yet
Do:
 * Carry on with the exercises as instructed by your physiotherapist * Carry on with the exercises as instructed by your physiotherapist
* Take regular short walks
* Keep walking with your walking aids until 4-6 weeks after your operation. You will then progress to 1 stick held in the opposite hand to your new hip
* Stand and sit as shown in hospital - operated leg in front, push on the arms of the chair, bed mattress or toilet seat frame
  * Avoid pressure on the wound until it has fully healed * Avoid pressure on the wound until it has fully healed
* Avoid picking up objects from the floor or reaching down, unless you have been shown the correct method by
the Therapist. Do not reach for objects when sitting -use a ĎHelping Handí for small objects. You will be given
one on loan if you live alone.
* Go to your GP if you have an unusual pain, temperature, notice a discharge from your wound or any pain
or swelling in your calves
* Ensure you take regular pain-killers for as long as you need to
Donít:
 * Twist the operated leg in or out whilst sitting or standing for at least 3 months * Twist the operated leg in or out whilst sitting or standing for at least 3 months
* Cross your legs, knees or ankles for at least 3 months
* Lift the knee of your operated leg higher than your waist/hip or bend your body down onto your thighs
* Sit on low chairs, stools or toilets
* Try to cut your own toe nails, put your shoes on without a long handled shoe horn, or take off/ put on your TED stockings - GET HELP
* Drive a vehicle until advised it is safe to do so  
 * Do any heavy lifting, housework or gardening * Do any heavy lifting, housework or gardening
* Discard any walking aids until advised to do so
* Do too much too soon - gradually increase your activities as able
* Return to work or sporting activities until advised to do so
Community Intermediate Care
The Community Intermediate Care Team is a team of Qualified Nurses, Health Care Support Workers and Therapists who can support your early discharge home following your hip replacement.
The Community Intermediate Care Team can support the early transfer of care from hospital to your own home, for a period of recovery, recuperation and rehabilitation. They will provide the most appropriate care package for you, tailored to your individual needs, for up to 7 days.
With your initial consent, a co-ordinator will visit you at home between your pre-operative assessment and your date of admission to discuss the service with you and gain your agreement for supported early discharge.
The team also works very closely with other colleagues in the community, such as District Nursing teams and Social Services and will liaise with these services if you require ongoing care and support in your own home.
When You Go Home
It is important to continue with your exercises. The success of the operation has a lot to do with how well you do your exercises and strengthen your muscles. This part of your recovery is very much down to you.
If excess muscle aching occurs, cut back on your exercises but do not stop.
Wound stitches or staples are removed on about the twelfth day after surgery. The Community Intermediate Care Team will arrange for a District Nurse to visit you in your own home.
Using stairs
Before discharge home you will be shown how to go up and down stairs. Even if you live in a flat or a bungalow, it is a good idea to practice while in hospital, as it allows you to go out and visit friends, without worrying about managing kerbs or steps.
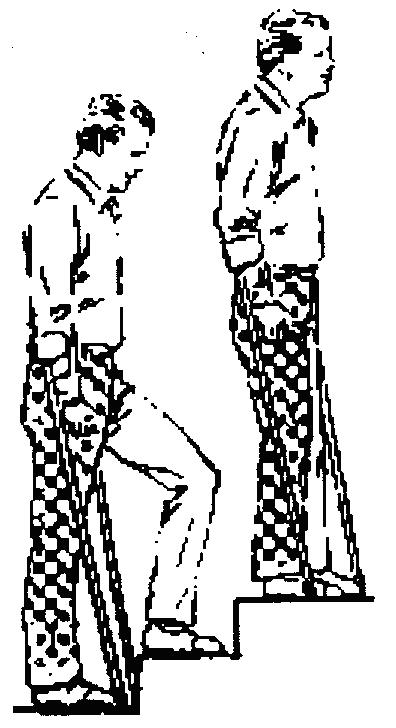 Going up - Move your good leg first, then your new hip and sticks Going up - Move your good leg first, then your new hip and sticks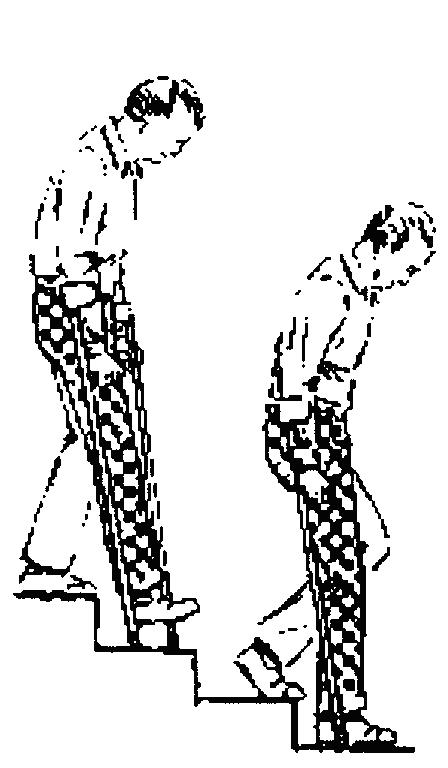
Going down - Sticks first, then new hip followed by good leg
In bed
 It is best to lie on your back for the first 6 weeks. You may be advised to keep a pillow between your legs to prevent them from crossing. Do not lean forward to pull up your bed clothes. It is best to lie on your back for the first 6 weeks. You may be advised to keep a pillow between your legs to prevent them from crossing. Do not lean forward to pull up your bed clothes.
Resuming sexual intercourse
It is advisable to refrain for 6-8 weeks following surgery and then to remember to avoid bending your hips.
Bathing
It is recommended that you do not get into the bath for at least 6 weeks following your hip replacement as this can put excessive strain on the new joint.
A strip wash is recommended or you may use a walk-in shower with assistance once your stitches have been removed, as long as there are no steps into the shower.
Getting in and out of the car
 When getting into a car, have it parked away from the kerb so that you do not have to stoop too low to get in. When getting into a car, have it parked away from the kerb so that you do not have to stoop too low to get in.
Have the seat adjusted as far back as it will go and recline the backrest. Sit sideways on the seat first, then keeping your operated hip straight, slowly swing your legs into the car so that you are facing the front. A glossy magazine or plastic bag on the seat helps you turn in the seat.
Avoid bending your hips more than 90 degrees or raising your knee higher than your hip. If the seat is too low, you may need a cushion or pillow to raise you a little.
Prevention of infection
If at any time after surgery you develop an infection, you need to visit your family doctor. For example if you develop a urine infection, tooth or gum infection, infected cut or boil. He may decide you need a course of antibiotics. Viral infections like colds are not a problem.
Dental work can sometimes release bacteria into the bloodstream. Always tell your dentist that you have had a hip replacement. He may decide you need a course of antibiotics.
When Do I Return To Clinic?
Your first appointment is approximately 6 weeks after discharge from hospital. The ward staff will make this appointment for you before you are discharged from hospital. At this appointment you will be examined and given advice on the long-term management of your new hip.
Partners in Care
We want you to be our partner in care. Please try to help by:
* providing full information on your health history and related matters;
* following the advice given to you;
* accepting responsibility if you refuse treatment or medical advice;
* taking reasonable care of your own property and respecting the property of other people in
hospital;
* keeping appointments and giving adequate notice if unable to do so;
* switching off your mobile phone when in hospital;
* not smoking;
* ensuring reasonable and responsible behaviour by yourself and your visitors;
* return any equipment when you have finished with it.
If you have any questions, which are not answered by this leaflet, then please donít hesitate to ask your doctor or one of the nursing staff.
|